Table of Contents
ToggleAccidents happen, and when they do, burns can turn a fun day into a sizzling disaster. Whether it’s a kitchen mishap or a sunbathing session gone wrong, knowing what to put on a burn can make all the difference. It’s not just about treating the burn; it’s about saving your skin and your sanity.
Understanding Burns
Burns occur when skin or underlying tissues suffer damage from heat, chemicals, radiation, or electricity. Various types of burns include first-degree, second-degree, and third-degree burns, with each requiring distinct treatment approaches.
First-degree burns affect only the outer layer of skin, often resulting in redness and pain. These burns typically heal within a week without scarring. On the other hand, second-degree burns impact deeper layers, causing blisters and significant pain. Healing can take several weeks, often leaving scars. Third-degree burns, the most severe type, damage all skin layers, potentially affecting muscles, tendons, or bones. Immediate medical attention is crucial for third-degree burns.
Common causes of burns include scalding from hot liquids, contact with flames, or exposure to chemicals. Skin is particularly vulnerable in the kitchen or during outdoor activities. An understanding of burn severity enables individuals to assess the situation accurately and seek appropriate treatment.
Recognizing symptoms plays a critical role in burn care. Signs of infection in burns may include increased redness, swelling, or pus. This awareness supports timely medical intervention, aiding in proper recovery.
Identifying appropriate treatments is essential for effective care. Cooling the burn with running water for 10 to 20 minutes serves as a primary first aid step. Over-the-counter pain relief medications can alleviate discomfort. Application of sterile bandages protects the area from further injury.
Ultimately, understanding burns and their treatment fosters a proactive approach to safety and health. Having essential knowledge empowers individuals to respond calmly and effectively, minimizing complications from burn injuries.
Types of Burns
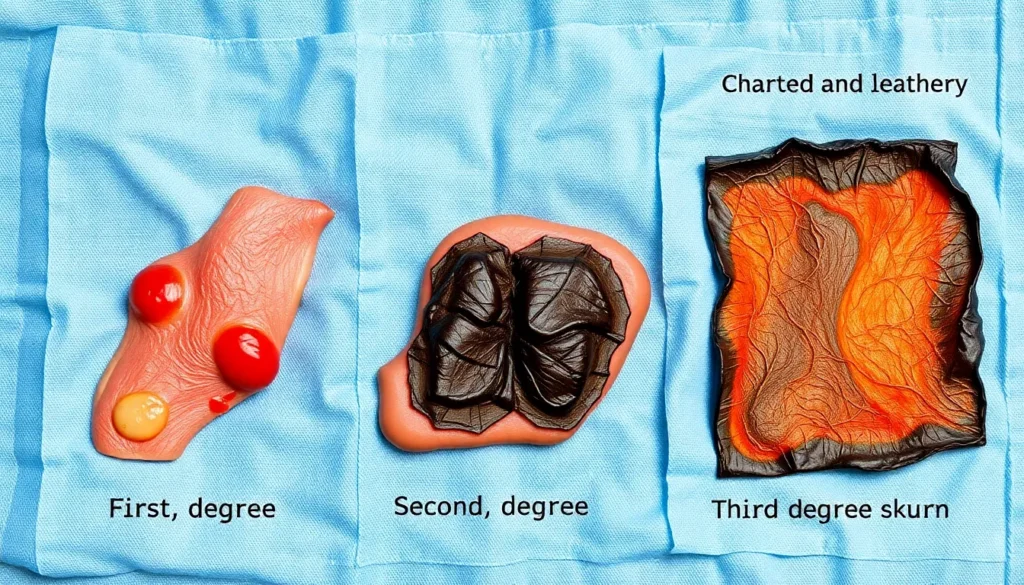
Burns are categorized based on severity and depth of skin damage. Understanding these types helps in selecting appropriate treatments.
First-Degree Burns
First-degree burns impact only the outer layer of skin, known as the epidermis. These burns cause redness, minor swelling, and pain. Typically, they heal within a week with minimal intervention. Symptoms often resolve without causing scars. Common causes include sunburn and brief contact with hot surfaces. Effective treatment involves cooling the burn with running water, applying soothing aloe vera, and covering it with a sterile bandage.
Second-Degree Burns
Second-degree burns affect both the epidermis and the underlying layer, called the dermis. These burns present with blistering, intense pain, and significant swelling. Healing time varies from two to three weeks, and there is a potential for scarring. Scalding from hot liquids and severe sun exposure often results in second-degree burns. Treatment includes cooling with water, protecting blisters, and using antibiotic ointments under a bandage to prevent infection.
Third-Degree Burns
Third-degree burns are the most severe, damaging all layers of skin and possibly affecting underlying tissues. Symptoms include charred, white, or leathery skin, and these burns can cause numbness due to nerve damage. Healing may take months, often requiring medical intervention such as skin grafts. Common causes include prolonged exposure to flames or electrical burns. Seeking immediate medical attention is crucial for proper treatment and recovery.
Initial Steps for Burn Treatment
Initial burn treatment is critical for effective healing and prevention of complications. Implementing proper steps immediately after a burn can significantly impact recovery.
Cool the Burn
Cooling the burn provides essential relief and mitigates tissue damage. Run cool (not cold) water over the affected area for 10 to 20 minutes. Alternatively, applying a cool, wet compress can also help. Avoid ice, as it may cause further skin damage. Cooling reduces inflammation and alleviates pain. Patients often notice a decrease in discomfort within minutes after following this step. Immediate cooling is especially important for second-degree burns to lessen blister formation.
Clean the Area
Cleaning the burn area prevents infection and promotes healing. First, gently cleanse the skin with mild soap and water. Pat the area dry with a clean towel, avoiding any scrubbing or friction. Routine cleaning can significantly decrease the risk of contaminants entering the wound. If blisters are present, do not pop them; they serve as a protective barrier. Proper hygiene practices during this step are crucial in ensuring a smooth healing process. Regular monitoring of the wound is important after cleaning to identify any signs of infection.
What to Put on Burn
Effective burn treatment involves using the right remedies. Selecting appropriate options minimizes pain and promotes healing.
Over-the-Counter Remedies
Over-the-counter (OTC) remedies provide immediate relief for minor burns. Products containing lidocaine can numb the affected area, helping to alleviate pain. Additionally, hydrocortisone cream reduces inflammation and soothes irritated skin. Antibacterial ointments such as bacitracin protect the burn from infection while keeping it moist. Sterile gauze pads act as a protective barrier, preventing further injury. Always clean the burn before applying any OTC products to ensure optimal results.
Natural Remedies
Natural remedies offer an alternative for burn care. Aloe vera stands out as a popular choice, known for its soothing properties and ability to promote healing. Applying honey acts as a natural antibacterial agent, which helps prevent infection. Coconut oil contains fatty acids that moisturize the skin and aid in healing. Lavender essential oil provides calming effects, reducing pain and inflammation. Chamomile tea bags, when cooled and applied to the burn, offer relief due to their anti-inflammatory properties.
When to Seek Medical Attention
Recognizing when to seek medical attention for burns is essential for proper healing and preventing complications. Visit a healthcare professional if a burn exceeds three inches in diameter, as larger burns may require specialized treatment. Seek immediate care for second-degree burns located on the face, hands, feet, genitals, or over major joints, as these areas are critical for function.
Consulting a physician becomes necessary if blisters develop and show signs of infection, such as increased redness, swelling, or discharge. Notably, third-degree burns demand emergency treatment, as they destroy all layers of skin and can lead to severe complications. Symptoms like charred or leathery skin indicate significant tissue damage requiring urgent medical intervention.
Watch for persistent pain that does not improve with over-the-counter pain relievers, signaling possible deeper injury or infection. If a person experiences any systemic symptoms, such as fever or chills, contacting a healthcare provider becomes crucial. Individuals with pre-existing conditions like diabetes or compromised immune systems should also seek medical evaluation sooner to prevent complications.
Burns caused by chemicals or electricity should receive professional assessment immediately, regardless of severity. Damage from these sources may not be visible externally but can affect deeper tissues. Lastly, emotional distress following a burn incident can also prompt a need for psychological support, especially after severe injuries.
Prevention Tips for Burns
Avoiding burns requires attention and care in potentially hazardous environments. Wearing protective gear, such as oven mitts while cooking or sunscreen when outdoors, significantly decreases burn risk. Installing safety measures like temperature regulators on faucets can prevent scalding hot water injuries.
Educating children about hot surfaces, sharp objects, and boiling liquids will build their awareness of burn dangers. Keeping hot liquids out of reach of children creates a safer home environment. Cooking at lower heat settings and using back burners can further minimize accidental splashes and spills.
Monitoring outdoor activities during peak sun hours helps reduce the chances of sunburn. Seeking shade or wearing hats and long sleeves offers additional protection from UV rays. Furthermore, using broad-spectrum sunscreen with an SPF of at least 30 enhances skin safety against sun damage.
Inspecting electrical appliances and cords for wear or damage reduces the risk of electrical burns. Unplugging devices when not in use also promotes safety. Always following the manufacturer’s instructions when using heated tools, like curling irons or soldering devices, is crucial for safe handling.
In the workplace, implementing safety protocols related to heat sources and chemicals provides additional layers of protection. Training staff on burn prevention and installing appropriate safety equipment further enhances safety standards.
Keeping a first-aid kit stocked with burn treatment supplies ensures readiness for minor burns. Understanding burn prevention is key to promoting safety and health in various environments.
Knowing how to treat burns effectively can make a significant difference in recovery and overall skin health. By following the initial steps of cooling the burn and applying appropriate remedies, individuals can alleviate pain and reduce the risk of complications.
Recognizing when to seek medical attention is equally important, especially for more severe burns or signs of infection. Proactive measures can prevent burn incidents and ensure safety in everyday situations.
With the right knowledge and tools, anyone can respond to burn injuries calmly and confidently, promoting healing and peace of mind.







